Lymphedema 101:
What is it and What can I do about it?
By: Dr. Shirlea North, PT, GCS, CLT

As I write this blog, it is March and International Lymphedema Awareness Month. Just like many conditions that are under-diagnosed, Lymphedema deserves more awareness and more education to health care providers and the public.
First, we need to answer the question “what is lymphedema”? To answer this simply, lymphedema is an accumulation of a protein-rich fluid that is outside lymphatic vessels. There is primary or congenital lymphedema and secondary lymphedema. Primary lymphedema can be caused by a reduction of lymph nodes present in the body or an inefficient lymphatic system. This presents with unilateral or one-sided involvement with either the upper or lower limb. Secondary lymphedema is typically caused by systemic infection, often post-surgical. This can occur after the removal of lymphatic vessels or nodes or nodes effected by chemo or radiation treatment for clients with cancer. Sometimes, this type of lymphedema could also be caused from a physical block to lymphatic flow which is found in those with lipedema (check out my other blog 😉 for more information). Secondary lymphedema, if left untreated, can develop into major medical issues like mobility difficulties and risk of infection.
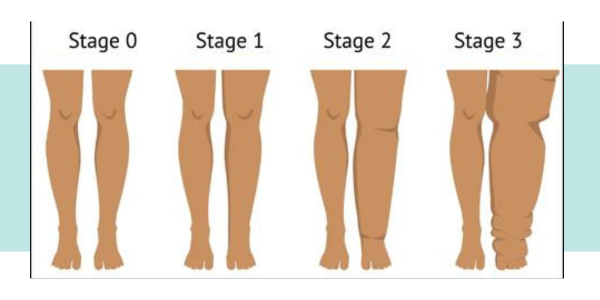
Both types of lymphedema have the fluid accumulation that is actually outside of lymphatic vessels and superficially or right underneath the skin. That is why more progressed stages causes skin changes like redness, blisters, hardening, and weeping wounds. These present as a huge risk of infection. There are stages to lymphedema that can be defined clinically:
Stage 0: (Latency) subclinical presentation with a sense of fullness, heaviness, or diffuse tingling of the limb without external edema or swelling or skin changes. *Communicating these symptoms to your provider and being assessed by a certified lymphedema therapist (CLT) can assist to prevent any further progression.
Stage 1: (Spontaneously Reversible) edema or swelling that is intermittent or come and go. Elevation of the limb helps with reduction.*This is a great time to seek an assessment and treatment for self-management tools that can help prevent any further exacerbation as this stage can quickly progress to stage 2.
Stage 2: (Spontaneously Irreversible) Edema is more prevalent and obvious with signs of skin changes with less pitting and firmer tissue that forms into fibrotic tissue from the stagnant lymph fluid. *Seeking treatment from a CLT is imperative in this stage to reduce limb volume and improve tissue integrity and will require more intensive or frequent treatment and being more vigilance for follow-up.
Stage 3: (Lymphostatic Elephantiasis) often what people think of first with lymphedema. Here is where the skin becomes very hard, fibrotic, can develop into breakdown with weeping sores and could cause irreversible damage if left untreated. There is also significant risk of infection that could spread systemically. *This absolutely requires collaboration with a CLT to resolve skin issues and limb volume and requires an intensive phase of treatment with maintenance program and periodic follow-up.
All forms of lymphedema can be treated conservatively upon visit with CLT. There are more drastic measures and surgical interventions that include lymph node transfers and debulking procedures, however that is to be carefully considered and should not be the first line of treatment.
As a CLT and physical therapist, I must perform a comprehensive examination of the individual’s movement and their personal goals as well as to educate and advocate for their entire lymphatic system. CLTs are trained and skilled healthcare professionals, often physical, occupational or massage therapists who implement the Complete Decongestive Therapy or Treatment (CDT) method. This includes manual lymphatic drainage (MLD) techniques, multilayer compression bandaging, elevation, mobility, skin/nail care, possible wound management if needed. It will also assist with transition from intensive phase to maintenance with compression garments, self-MLD techniques, possible use of sequential pneumatic compression pump, and continued progression of mobility exercises and skin/nail care.
Lymphedema is a chronic and potentially progressive condition; however, it is not what defines the individual and should not limit or reduce their quality of life. To take care of your lymphatic system is one of the best ways to take care of your body with lasting effects.
Northstar Academy Resources
Check out my Lymphatic Wellness E-book where it dives a bit deeper into the conservative measures that you can start today!
Northstar Academy Resources
Check out my Lymphatic Wellness E-book where it dives a bit deeper into the conservative measures that you can start today!
Northstar Podcast
Follow me on my podcast, NorthStar Physical Therapy for quick, realistic and down-to-earth education and evidence based medical information on lymphatic conditions, lipedema, pelvic health conditions and chronic and progressive neurological conditions like Parkinson’s, stroke and Multiple Sclerosis.







